
Communications Technologies as Community Technologies: Alaska Native Villages and the NASA Satellite Health Trials of the 1970s
Technology’s Stories vol. 5, no. 2 – doi: 10.15763/JOU.TS.2017.5.2.02
PDF: LanzarottaGreene_Communications Technologies
In May 1975, high above the earth’s surface, a structure resembling a large mushroom with two snow shovels attached to its dome released itself from stable geosynchronous orbit and drifted to a new station over Lake Victoria in Central Africa. The passage of the NASA Applied Technology Satellite 6 (ATS-6) from the Western Hemisphere to the Eastern Hemisphere marked the conclusion of a set of innovative trials that used satellites as healthcare delivery tools for remote villages in the Alaskan interior.[1] Two other partners in these trials, the Indian Health Service and the Lister Hill Center for Biocommunications (a new division of the National Library of Medicine) hoped that the satellite would both establish them as global innovators in health communications technology, and draw attention to how marrying high-tech with low-tech solutions could enable community health workers to build primary care networks in remote areas.
In a series of essays covering the project, the journal Spaceflight referred to ATS-6 as a “Community Satellite” that could be used with inexpensive ground modules to create communications infrastructure in remote and resource-poor regions.[2] An internal NASA report claimed that the “versatile spacecraft climaxes NASA’s ATS program that, since 1966, has been advancing the frontiers of knowledge…[and] demonstrating how widespread applications of presently available technology could contribute to lessening ignorance, poverty, and inadequate health care… worldwide.”[3] This project came at a crucial moment in NASA’s history, as the agency’s funding was increasingly contingent on demonstrating the application of their technologies for domestic infrastructure and U.S. foreign aid.[4] Beginning with the first ATS satellite (ATS-1) in 1966, NASA had used Alaskan communities to prove that communications technologies could also be technologies of health and development.
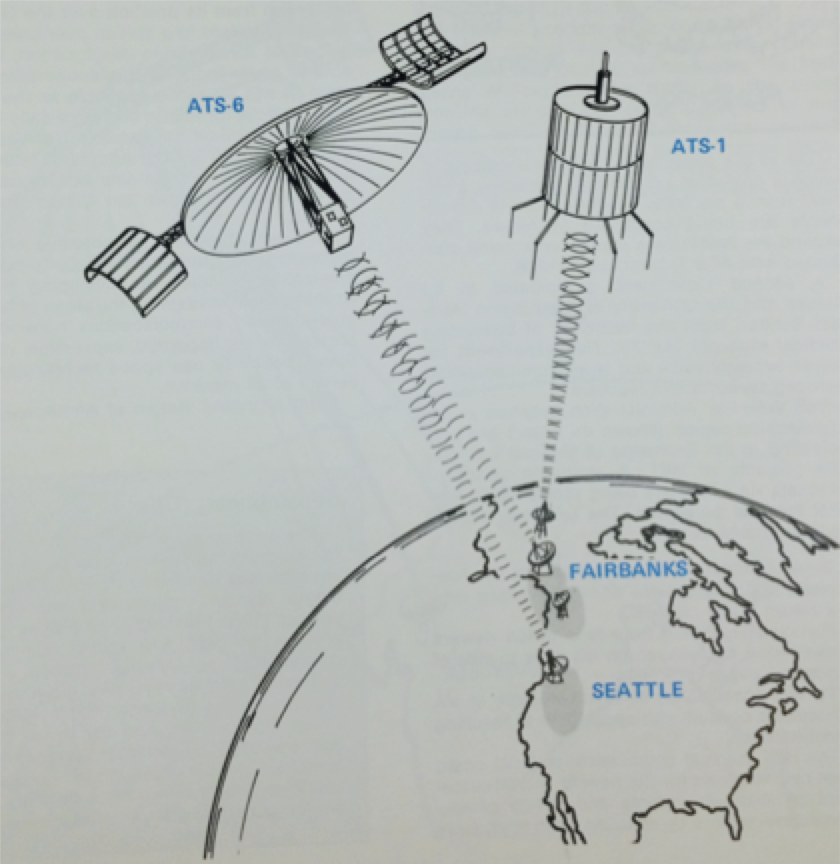
Figure 1. The ATS-1 (1966) and ATS-6 (1974) satellites linked communications over the Arctic. Source: Health–Education Telecommunications Experiment (HET): A Cooperative Project [HEW/NASA].
Throughout the Cold War, various federal agencies had tried to use large-scale technological interventions to expand Alaska’s military and industrial capacities. Anxious that the Soviet Union might target Alaska, the U.S. government entered a bilateral agreement with Canada to construct the Distant Early Warning Line, a series of radar stations, along the Alaskan coast.[5] In the late 1950s, the Atomic Energy Commission (AEC) even planned to detonate two atomic bombs in order to create an arctic harbor at Cape Thomson. They claimed that such a harbor would benefit Alaska’s long-term economic development and create new opportunities for its indigenous peoples.[6] When one AEC official was asked to comment on the impact that this program would have on the communities who hunted and fished around Cape Thomson, he explained: “We are not interested in preserving the Eskimo as a hunter, we are interested in giving him the opportunity of becoming a coal miner.”[7] Soon thereafter, however, the Iñupiat of nearby Point Hope vehemently opposed the plan and successfully pressured the AEC to abandon it.[8] By the 1970s, then, Alaska Native peoples were far from naïve about the intentions of federal agencies that proposed high-tech infrastructural projects.[9]

The DEW line station at Point Barrow as it appeared in 1996. Note that the constructions of totem poles is not a traditional part of Iñupiat culture; the one seen here was erected by Army staff to celebrate the construction of the first flush toilet in Barrow. Source: Ruth A.M. Schmidt Papers, Archives and Special Collections Library, University of Alaska Anchorage.
The story of the ATS experiments is not simply another instance of a federal agency using Alaska as a site to pursue a broader Cold War strategy. Alaska Native leaders and rural healthcare workers embraced satellites as tools that could help preserve and extend the autonomy of their communities. In order to understand why they greeted these particular technologies so hopefully, we revisit an earlier set of health interventions through which Alaska Native communities encountered biomedical technologies. This essay, an early report from a broader collaborative project on histories of health and technology in Alaska, focuses on how the disruption and trauma of forced hospitalization—simultaneously a problem of medicine, technology, and geography—was a key issue that satellites were poised to help resolve.
Tuberculosis and the Trauma of Hospitalization
By the 1940s, Alaskan health officials had identified tuberculosis as the most pressing health concern in the Alaska Territory. However, the lack of robust public health infrastructure, turned even basic tasks such as assessing the true extent of the problem into a major challenge. In response to these issues, the Territorial Department of Health acquired decommissioned naval vessels, which could travel to remote communities along the coast and up the Yukon River.[10] The staff of these ships provided some limited medical care, but their primary purpose was to perform diagnostic x-rays and generate data on tuberculosis rates.
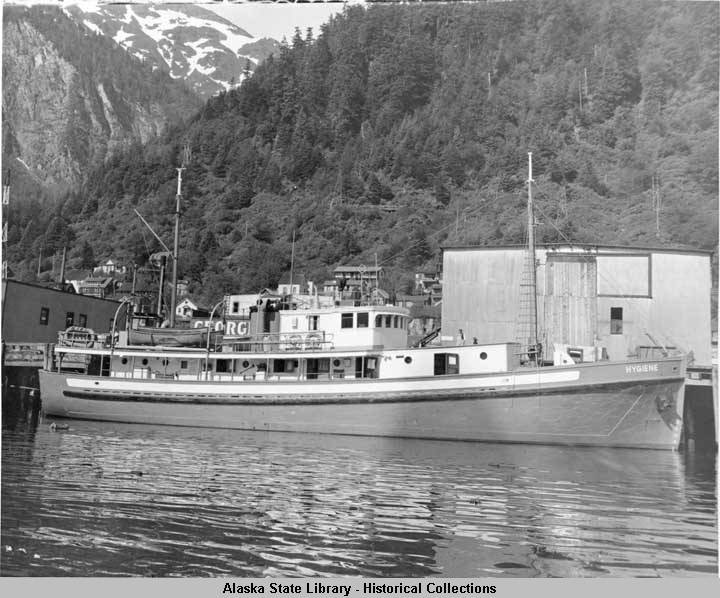
The M/S Hygiene at dock in Juneau. Source: Alaska State Library, Alaska Department of Health and Social Services Collection, Photo by William L. Paul, Jr., ASL-P143-0292
Their preliminary findings convinced the Department of the Interior to sponsor a more comprehensive report, released in 1954. The results were shocking: tuberculosis was responsible for more than a third of deaths amongst Alaska Native peoples.[11] The report suggested that the hundreds of tuberculosis patients awaiting hospital beds in Alaska should immediately be sent to sanitariums in Washington State.[12] In the course of implementing this plan, the Department of Health circulated encouraging pamphlets that portrayed hospital life as restorative, or even idyllic, in Alaska Native communities.[13] However, their promotional literature belied darker realities about the experience of hospitalization for patients and for their families.

Airlift of T.B. patients, August 16, 1954. Source: Alaska State Library, Alaska Department of Health and Social Services Collection, Photo by Robert Campbell Reeve, ASL-P143-00095.
As anthropologist Lisa Stevenson has described in her study of the Canadian Arctic, removing indigenous patients from their communities and relocating them to distant tuberculosis hospitals proved traumatic for both patients and their families.[14] In the 1950s, U.S. Public Health Service anthropologists traveled to Seattle hospitals to interview “Eskimo” patients and observed a similar pattern. Alaska Native patients were often depressed and consumed by the fear that hospitalization amounted to “going away to die among strangers.” They struggled to contact their families, resulting in considerable anxiety, and found communicating with English-speaking hospital staff difficult and frustrating.[15] These experiences would be remembered as violent displacements, which fractured communities, dehumanized patients, and forced assimilation.[16]
Keeping Care in the Village
A later tuberculosis intervention was received more favorably. By the end of the 1950s, the Department of Health also developed an ambulatory chemotherapy program, which employed field nurses to visit villages every few months to replenish supplies of new and experimental tuberculosis drugs.[17] Each village also chose a chemotherapy aide, who was responsible for overseeing the program day-to-day by taking patients vital statistics and distributing medications and vitamins.[18] The program was popular—in at least one village, the local government heard of it over the radio and asked to be enrolled.[19] Within five years, hospitalizations were in steep decline.[20]
From the point of view of health officials, this experience justified training indigenous health aides. After visiting the village of Emmonak in 1956 and enlisting the help of local health aides to run a temporary clinic, Dr. Walter Johnson observed that they “could make observations as well as any physicians.”[21] Convinced that rural medical care should be provided by “a local person who did not leave after a couple of years (like teachers often did) and who spoke the same language as the patients,” Johnson became a staunch advocate for the creation of a statewide community health aide program employing Alaskan natives as health workers in situ.[22]
After several regional programs demonstrated success using health aides, Johnson convinced the directors of the regional Public Heath Service units that health aides should be a key feature of Alaskan rural health. The program gradually expanded throughout the 1960s, receiving a significant boost due to President Johnson’s creation of the Office of Economic Opportunity (OEO), which had a mandate to increase “community participation” in indigenous healthcare programs. In the wake of the 1971 Alaska Native Claims Settlement Act, Alaska Native regional corporations increasingly took control of their own healthcare, and were able to secure grants from the OEO to further develop their community health aide programs.[23]
Satellites and Self-Determination
In 1971, the Director of the Alaska Area Native Health Service, John F. Lee, boasted the success of the health aide program by noting the irony “that in this age of technological sophistication one of the most important advances in improving health services to remote villages… the Native village health aide.”[24] Lee recognized the need for telecommunications technologies; many inland villages lacked regular telephone, or even radio, contact. He was hopeful that satellites, while only “in use on an experimental basis,” would soon provide a solution.[25]

Schoolhouse and satellite radio direction beam in Anaktuvuk Pass, 1972. Source: Ruth A.M. Schmidt Papers, Archives and Special Collections Library, University of Alaska Anchorage.
Lee was referring to the ATS-1 , initially launched in 1966, which he and the other project designers hoped could be adapted to improve rural health services, now that its original projects were complete. But others involved in the assessment of rural healthcare voiced qualms: what if satellite telecommunications made remote communities more dependent upon outside physicians and less able to function independently? A group of Stanford researchers on the project elaborated on this concern:
The villages are places of contrast. Airplanes are used by people who fish for subsistence; satellite radio transceivers are placed in houses where the heating comes from metal barrels transformed into fireplaces… Either these contrasts will be absorbed in a synthesis of the traditional and the modern… [Or they will] end the originality and values of their distinctive civilization… It is of basic importance to supply the necessary social services to the population… without side effects that will increase the dependency of the community…[26]
The central Tanana Region for the ATS-1 experiment was chosen (probably by decision makers from Alaska Native Health Board, the Indian Health Service, and the Lister Hill Center for Biomedical Communication at the National Institutes of Health) because of its low population density and poor telecommunications infrastructure. The nine communities selected as “experimental villages” received bulky ground stations that connected health aides with the Tanana Hospital (staffed by a doctor) and Fort Yukon Hospital (staffed by a registered nurse), and with the Alaska Native Medical Center in Anchorage. These “experimental villages” were compared to five “control villages” without ground stations.
By the end of the study, health aides in six of the nine “experimental villages” could list specific examples of diagnostic information or therapeutic techniques they had learned over the radio. None of the health aides in control villages could offer similar examples.[27] Furthermore, being more closely connected to remote physicians did not seem to create greater dependency. Physicians involved in the project reported that only 0.5% of calls were particularly severe, and that half the time the health aide’s plan as stated would have required no supervision.[28]
For instance, the transcript of a conversation between health aides and physicians reproduced below shows that the former acted autonomously, checking in with physicians simply to confirm their treatment plans:
VILLAGE HEALTH AIDE: Day before yesterday, (male patient) age 7, was playing in the yard, schoolyard, and fell… His arm was kind of hanging so I start feeling around and he looked like he had a broken collar bone so I put a bigger ace bandage on it and yesterday, I checked it, it was loose, I tightened it again and he’s doing OK, I check him this morning—he was OK, over.
TANANA PHYSICIAN: OK, that’s fine, make sure that they understand that the figure of eight needs to stay on… until the collarbone is non-tender—so that you can push around and it doesn’t hurt… He’ll need to wear it for a number of weeks probably at least 3, over.
VILLAGE HEALTH AIDE: Roger, Roger. That’s what I told the mother that it should be on at least 3 weeks.[29]
The Stanford research team produced a film on the ATS-1 experiment, Satellite House Call, which echoed some of the claims of the project’s designers in an effort to demonstrate the value of satellite healthcare to state and federal agencies. The narrator, is the prominent Alaska Native activist and politician William “Willie” Iġġiaġruk Hensley. He explained that village residents still lived according to tradition. And yet, he added, “in other ways, they are leading emerging nations into the next century. The Alaskan bush is a developing nation itself!”[30]




Screenshots from Satellite House Call
Much of the film focused on Bertha Moses, a community health aide in the village of Allakaket. Before the satellite, she recalled, it was difficult to reach the Tanana hospital, which had sometimes left her feeling “helpless,” but with the satellite link she could communicate daily with a physician, which gave her “more confidence” in the treatment she provided.[31] Family members, as well, could now maintain contact with their sick relatives who were receiving treatment in Tanana or Anchorage. In the words of one village resident: “Last year (before satellite) we didn’t know if they were dead, still in hospital, or what.”[32] In communities where hospitalization had previously meant
complete isolation, this was an extraordinarily important change. By 1973, the Tanana Chiefs Conference, the organization responsible for coordinating health services in the region, requested additional ATS-1 ground stations for those villages still lacking reliable communications technologies.[33]
Telemedicine and its Limitations
ATS-1 was intended to be a brief demonstration project, and it had not been designed to orbit perpetually. Its success, as the Stanford research team pointed out, left the Indian Health Service and the project’s designers, “with a severe moral problem.” How could they end the trial without providing a replacement? “The native communities,” the Stanford team explained, “have been given much higher expectations concerning appropriate standards of service.”[34]
With no way back, the Indian Health Service sought a path forward. The positive results of the ATS-1 experiment coincided fortuitously with the development of ATS-6, the “community satellite,” and its smaller and cheaper ground stations. [35] Unlike ATS-1, ATS-6 was developed with health communications in mind. It was conceived partly as the vessel for a broader “Health-Education Telecommunications Experiment,” developed jointly by NASA and the Department of Health Education and Welfare.[36] Alaska was identified as an ideal site to test the satellite and the emerging modality of “telemedicine,” a term coined in 1972 to describe the addition of interactive television to long-distance medical practice.
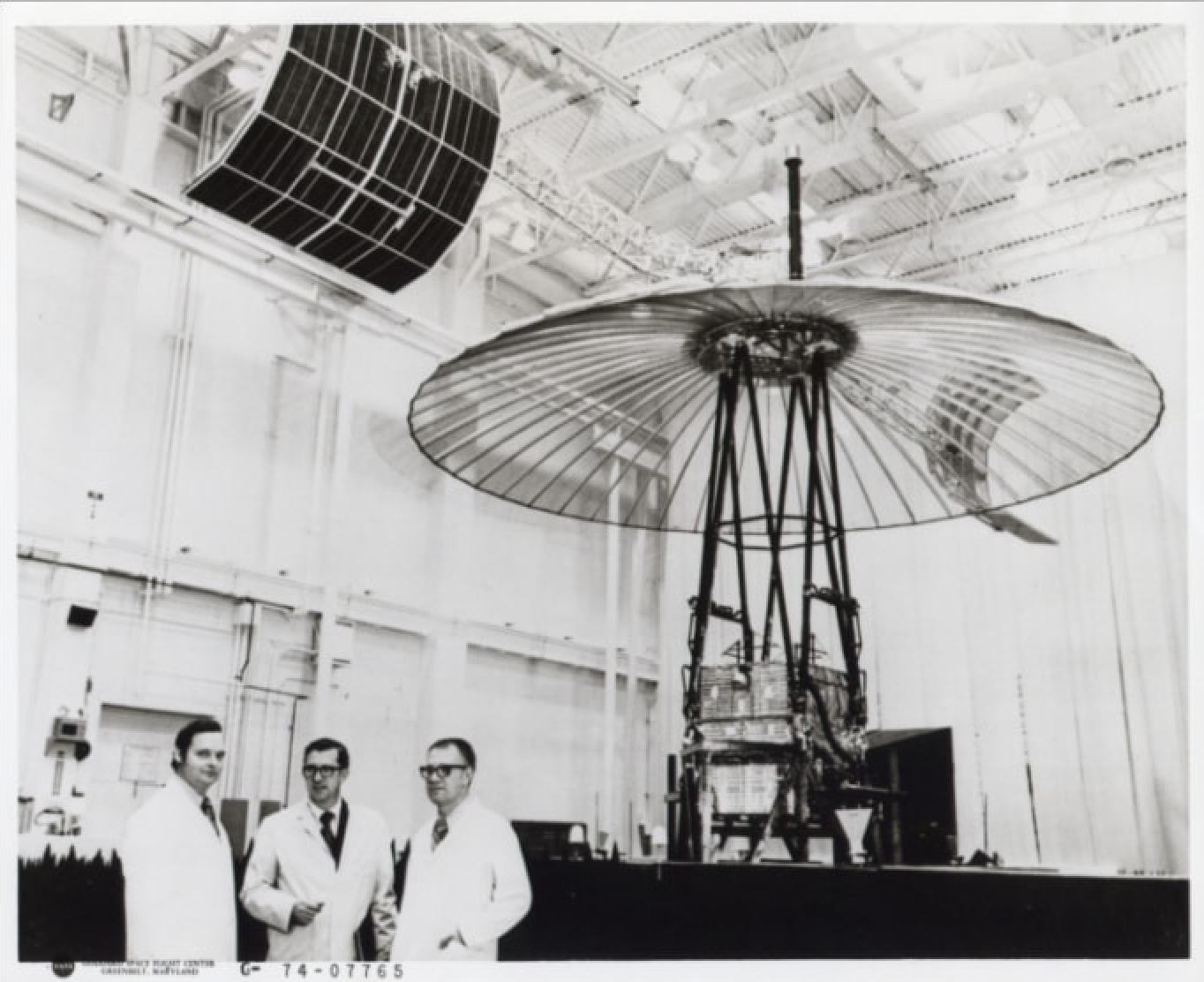
The ATS-6 under development. Source: NASA. https://www.nasa.gov/centers/goddard/missions/ats.html
The U.S. Department of Health, Education, and Welfare, along with NASA, had become interested in the potential of interactive television to improve access to healthcare. By early 1974, it had funded 13 telemedical demonstration programs, each of which was designed to harness the liberatory potential of television to address disparities in healthcare access. Tanana again served as an arena to test whether satellite telemedicine could help physicians guide health aides and rural medics.[37] Alaskan villages (along with communities in rural Appalachia and India) would also serve as field sites to test new health information programming, a project that would dramatically increase the availability of television in rural communities.[38]
The results of ATS-6 “television medicine” trials were less conclusive than the ATS-1 “satellite radio” experiments. The ground stations were cheaper, so more villages could be included, but the benefits of adding television to medical communication were not as clear. Leaders of Alaska Native communities wondered if the risks of making television more broadly available in their communities—fostering young peoples’ dissatisfaction with village life and their desire to leave—might outweigh the benefits of telemedicine.[39]
Broader critiques of satellites as healthcare technologies also emerged. Some worried about developing communications systems that assumed spatial isolation was inevitable, instead of developing infrastructure that more effectively connected rural communities. A few years before ATS-6 was launched, Walter J. McNerney, the president of Blue Cross, expressed his reservations:
We have seen attempts made by industry to use its excess capacity in callous disregard of need. One example of that was the proposal made by a large company to put a satellite over Southwest Indian territory so that problems and treatment could be televised. This investment in technical equipment and personnel would be absurd in terms of population and simple primary care alternatives.[40]
However, officials from local non-profit organizations argued that the ATS-6, like other telecommunications technologies, was part of an investment in infrastructure. Who controlled the development of this infrastructure—and the degree to which it was understood as a public service or a private good—would remain an object of fierce contestation, especially in Alaska. For instance, in 1974, Robert J. Clark, the Deputy Director of the Bristol Bay Area Health Corporation, wrote to the Alaska Telecommunications Office with pointed questions: “Have you sent a person out to Bristol Bay in the past year to assess each village’s need? If not, why? Isn’t it your responsibility?” Clark had learned about the ATS program at a recent Rural Health Seminar hosted by the Alaska Federation of Natives, and urged that Alaska should act quickly to extend satellite telecommunications to include Bristol Bay.[41] Contrary to critics who viewed telecommunications satellites as a poor replacement for genuine health infrastructure, many rural Alaskans came to see these networks as a new form of medical infrastructure that could keep medical care, and patients, in their home villages.
Conclusion: Who and what are satellites for?
NASA’s ATS health trials positioned rural Alaska as an experimental space for testing applications of satellite telecommunications that could also be used to improve healthcare in the global South. In this context, Alaska could stand in for other developing regions where American technical expertise might become valuable. But Alaska Native political leaders and indigenous community health aides conceived the ATS-1 and ATS-6 as tools that could improve Alaska Native health without sacrificing the hard-won autonomy of their communities. These groups were motivated, respectively, by the desire to bring satellite technologies into their regions and the hope of integrating these technologies into their own local healthcare practices.
The presence of these disparate aims—which represent different visions of what health communications satellites might be able to do and whom they might do it for—existed within the same project. Alaska Native leaders understood there were risks, as well as benefits, in NASA’s interest in rural Alaska. At the same time, NASA, the IHS, Lister Hill, and Stanford were aware that there were risks, as well as benefits, in demonstrating that the ATS program could genuinely help respond to the healthcare needs of rural Alaskans.
Yet while all parties converged on positioning communications technologies as technologies linking community health and development, the meanings of “community health” would differ substantially, depending in part on whether that term was being invoked in the first or the third person. Unlike the technologies of health and surveillance deployed a generation earlier in the management of tuberculosis, which locals remembered as disruptive and coercive interventions, these early satellites trials are remembered by Alaska Native health workers as a key tool in a long struggle for self-determination.
Further material, including an archive of oral histories of the first generation of Alaska community health aides and the film Satellite House Call, can be found at the University of Alaska’s Project Jukebox.
Tess Lanzarotta is a Ph.D. Candidate in the History of Science and Medicine at Yale University. Her research focuses broadly on the history of biomedical research in Cold War Alaska, and on how contemporary interactions between researchers and Alaska Native peoples are shaped by their historical antecedents.
Jeremy A. Greene, M.D., Ph.D., is Professor of Medicine and the History of Medicine and holds the Elizabeth A. Treide and A. McGehee Harvey Chair in the History of Medicine at the Johns Hopkins School of Medicine; his most recent book, Generic: The Unbranding of Modern Medicines, was published by Johns Hopkins University Press. Greene’s first book, Prescribing by Numbers: Drugs and the Definition of Disease, was awarded the Rachel Carson Prize by the Society for the Social Studies of Science and the Edward Kremers Prize by the American Institute of the History of Pharmacy. He received an M.D. and a Ph.D. in the History of Science from Harvard University in 2005, finished a residency in Internal Medicine at the Brigham & Women’s Hospital in 2008, is board certified in Internal Medicine and a member of the American College of Physicians, and continues to practice primary care medicine in a community health center in East Baltimore.
Suggested Readings
Conway, Erik M. “Bringing NASA Back to Earth : A Search for Relevance during the Cold War.” In Science and Technology in the Global Cold War, edited by Naomi Oreskes and John Krige, 251-272. Cambridge: MIT Press, 2014.
Bashshur, Rashid L. Technology For Health. Washington, DC: Indian Health Service, 1980.
Bashshur, Rashid L. and Gary W. Shannon, History of Telemedicine: Evolution, Context, and Transformation. New Rochelle: Mary Ann Liebert Inc., 2009.
Fortuine, Robert. “Must We All Die?” Alaska’s Enduring Struggle with Tuberculosis. Fairbanks: University of Alaska Press, 2005.
Hudson, Heather E. Connecting Alaskans: Telecommunications in Alaska from Telegraph to Broadband. Fairbanks: University of Alaska Press, 2015.
Jones, David S. “The Health Care Experiments at Many Farms: The Navajo, Tuberculosis, and the Limits of Modern Medicine, 1952-1962.” Bulletin of the History of Medicine 76.4 (2002): 740-790.
Light, Jennifer S. From Warfare to Welfare : Defense Intellectuals and Urban Problems in Cold War America. Baltimore: Johns Hopkins University Press, 2003.
Stevenson, Lisa. Life Beside Itself: Imagining Care in the Canadian Arctic. Oakland: University of California Press, 2014.
Notes
[1] NASA, “Applications Technology Satellite-6,” NASA FACTS: An Educational Publication of the National Aeronautics and Space Administration.(Washington, DC: NASA, 1975); USAID, AIDSAT: Space Age Technology for Development (Washington, DC: USAID, 1976).
[2] “The Community Satellite-I.” Spaceflight, 1974, 340–50; “The Community Satellite-II.” Spaceflight, October 1974, 369–75; “The Community Satellite-III.” Spaceflight, December 1974, 423-440.
[3] NASA, “Applications Technology Satellite-6,” 1975, 2.
[4] Jennifer S. Light, From Warfare to Welfare: Defense Intellectuals and Urban Problems in Cold War America (Baltimore: Johns Hopkins University Press, 2003); Erik M. Conway, “Bringing NASA Back to Earth: A Search for Relevance during the Cold War,” in Science and Technology in the Global Cold War, eds. Naomi Oreskes and John Krige (Cambridge: the MIT Press, 2014), 251-272.
[5] On the militarization of Cold War Alaska, see Matthew J. Farish, “The Lab and the Land: Overcoming the Arctic in Cold War Alaska,” Isis 104:1 (2013): 1-29; John C. Reed and Andreas G. Ronhovde, Arctic Laboratory: A History (1947-1966) of the Naval Arctic Research Laboratory at Point Barrow, Alaska (Washington: Arctic Institute of North America, 1971). For resources on the history of the Distant Early Warning Line, see P. Whitney Lackenbauer, Matthew J. Farish, and Jennifer Arthur-Lackenbauer, The Distant Early Warning (DEW) Line: A Bibliography and Documentary Resource List, prepared for the Arctic Institute of North America (Calgary: Arctic Institute of North America, October 2005).
[6] Scott Kirsch, Proving Grounds: Project Plowshare and the Unrealized Dream of Nuclear Earthmoving (New Brunswick: Rutgers University Press, 2005); Scott Kaufman, Project Plowshare: The Peaceful Use of Nuclear Explosives in Cold War America (Ithaca: Cornell University Press, 2013).
[7] Quoted in Scott Kaufman, Project Plowshare: The Peaceful Use of Nuclear Explosives in Cold War America (Ithaca: Cornell University Press, 2013), 31.
[8] On the resistance to Project Chariot, see Dan O’Neill, The Firecracker Boys: H-Bombs, Inupiat Eskimos, and the Roots of the Environmental Movement (New York: BasicBooks, 2007).
[9] As Andrew Stuhl has recently pointed out, this pattern was particularly pronounced among the Inuit in Alaska and Canada, see Unfreezing the Arctic: Science Colonialism and the Transformation of Inuit Lands (Chicago: University of Chicago Press, 2016).
[10] Robert Fortuine, “Must We All Die?” Alaska’s Enduring Struggle with Tuberculosis (Fairbanks: University of Alaska Press, 2005), 76-81.
[11] Thomas Parran ed., Alaska’s Health: A Survey Report to the United States Department of the Interior (Pittsburgh: Graduate School of Public Health, University of Pittsburg, 1954), 83.
[12] Ibid., 237.
[13] “Dear Lucy” tuberculosis pamphlet. C. Earl Albrecht Papers, HMC-0375, Box 13, Folder 5, University of Alaska-Anchorage Archives and Special Collections.
[14] Lisa Stevenson, Life Beside Itself: Imagining Care in the Canadian Arctic (Oakland: University of California Press, 2014).
[15] Margaret Lantis and Evelyn N. Hadaway, “How Three Seattle Tuberculosis Hospitals Have Met the Needs of their Patients,” copy in M. Walter Johnson Papers HMC-0932, Folder 32, University of Alaska Anchorage Archives and Special Collections. In “Must We All Die?,” Robert Fortuine explains that there were rumors that physicians “threw away” the bodies of patients whose families could not afford to have them transported back to their villages. Decades later, it came to light that the bodies of deceased Alaska Native patients at a sanitarium on Sitka Island were stacked in abandoned WWII ammunition bunkers. This discovery has, understandably, resulted in renewed anger and grief for many who had been misled or left wondering about the fate of their relatives. Fortuine, Must We All Die?, 206. See “Remains of tuberculosis victims headed home,” Indian Country Today (July 19, 2000): C8.
[16] Fortuine, “Must We All Die?;” Lisa Stevenson, Life Beside Itself: Imagining Care in the Canadian Arctic (Oakland: University of California Press, 2014), tracks the trauma of these processes for those communities and the continuing trauma engendered by the impersonal models of healthcare implemented in Arctic communities.
[17] Fortuine, “Must We All Die?,” 138-139.
[18] Ibid., 140. For a contemporary description of the chemotherapy program, see Louis Lear, “Chemotherapy in Alaska,” American Journal of Nursing vol. 57, no. 3 (March 1957): 320.
[19] Fortuine, “Must We All Die?.”
[20] Ibid., 153.
[21] Walter Johnson, M.D., interviewed by Karen Brewster on 8 July 2005, H2004-17-06, Community Health Aides Program Project Jukebox http://jukebox.uaf.edu/CHA/htm/wjohnson1.htm. accessed 15 April 2017
[22] Walter Johnson, quoted in James P. Rife and Alan J. Dellapenna, Jr., Caring & Curing: A History of the Indian Health Service (Landover, MD: PHS Commissioned Officers Foundation for the Advancement of Public Helath, 2009), 50.
[23] Philip Nice with Walter Johnson, The Alaska Health Aide Program: A Tradition of Helping Ourselves (Anchorage: Institute for Circumpolar Health Studies, 1998), 16-40.
[24] John F. Lee, “The Challenges of Delivering Health Services to Rural Alaska Natives,” in Proceedings of the Second International Symposium on Circumpolar Health, Oulu, Finland, June 21-24 1971 (Stockholm: Laromedelsforlagen, 1972), 80.
[25] Ibid., 90.
[26] Osvaldo Kreimer et al., Health Care and Satellite Radio Communication in Village Alaska: Final Report of the ATS-1 Biomedical Satellite Experiment Evaluation (Palo Alto: Institute for Communications Research, Stanford University; Bethesda: Lister Hill National Center for Biomedical Communication, 1974), 16-17.
[27] Dennis Foote, Edwin B Parker, and Heather E Hudson, Telemedicine in Alaska: The ATS-6 Satellite Biomedical Demonstration (Palo Alto: Institute for Communication Research, Stanford University, 1976), 13.
[28] Kreimer, Health Care and Satellite Radio Communication, 9.
[29] Ibid., A-33.
[30] Satellite House Call, directed by Judy Irving (1975; Palo Alto: Stanford University Department of Communication), DVD. For more on the intentions behind the film, see Heather E. Hudson, Connecting Alaskans: Telecommunications in Alaska from Telegraph to Broadband (Fairbanks, University of Alaska Press, 2015). The film can be viewed in its entirety on the Community Health Aides Project Jukebox website.
[31] Satellite House Call.
[32] Kreimer, Health Care and Satellite Radio, 120.
[33] Heather E. Hudson and Edwin B. Parker, “Medical Communication in Alaska by Satellite,” The New England Journal of Medicine 289: 25 (1973): 1356.
[34] Ibid.
[35] Kreimer, Health Care and Satellite Radio, 217.
[36] Joel J. Reich, “Telemedicine: The Assessment of an Evolving Health Care Technology,” (Master’s thesis, Washington University-St. Louis, Center for Development Technology, 1974); Health –Education Telecommunications Experiment (HET): A Cooperative Project [HEW/NASA]: Experiment Summary Description (Washington, DC: NASA, 1974).
[37] Reich, “Telemedicine,” 69
[38] Chris Patricoski, “Alaska Telemedicine: Growth Through Collaboration,” International Journal of Circumpolar Health 63:4 (2004): 366.
[39] Dennis Foote, Edwin B Parker, and Heather E Hudson, Telemedicine in Alaska: The ATS-6 Satellite Biomedical Demonstration (Palo Alto: Stanford University, 1976). On contemporary concerns that TV may bring dissolution to Alaskan native life, see Norma Forbes, Television’s Effects on Rural Alaska: Summary of Final Report (Fairbanks: University of Alaska-Fairbanks, 1984); Daniel Cornwall, “Remember when TV came to Bush Alaska?” Alaska Daily News, April 8, 2009.
[40] Walter J. McNerney, “The Role of Technology in the Development of Health Institution Goals and Programs” in Technology and Health Care Systems in the 1980s, ed. M.F. Collen (Washington: Department of Health, Education, and Welfare, 1972), 166; quoted in Reich, “Telemedicine,” 205.
[41] Bristol Bay Native Association Records, HMC-0075, Box 2, Folder 23, University of Alaska-Anchorage Archives and Special Collections.
