Materializing Gender through Contraceptive Technology in the United States, 1930s–1940s
Technology’s Stories vol. 5, no. 1 – DOI: 10.15763/JOU.TS.2017.4.1.01
PDF: Drucker_Materializing Gender
This essay focuses on the intersection of gender, sexuality, and technology in the use of barrier methods (diaphragms and cervical caps) along with spermicides as contraceptive technologies in the 1930s and 1940s United States. Documents on contraceptive technologies in this era favor doctors’ perspectives, and highlight their understanding of the ways that female patients and their husbands used and responded to them. They also hint at the mixture of ambiguity, opportunity, and anxiety that these devices introduced into marriages. A specifically feminist perspective on contraceptive technology illustrates how “gender relations can be thought of as materialized in technology” in this era.[1]

Durex diaphragms, manufactured c. 1970. Image courtesy of the Royal College of Physicians and Surgeons of Glasgow (https://libraryblog.rcpsg.ac.uk/).
Contraceptive research in the Depression and World War II era demonstrates how a seemingly simple device like a barrier method could give rise to intricate reconfigurations of gender roles and behaviors. It shows how diaphragms and cervical caps materialized doctors’, patients’, and husbands’ ideas of femininity, women’s and men’s sexuality, and the medicalization of contraception. While doctors wanted to protect women’s health, they also aimed to enforce their own perceptions of what a healthy woman looked like. Manufacturers wanted to sell their own products and used medical expertise and patients’ concerns to do so.[2] What women and men using contraception in the first half of the twentieth century wanted themselves can be gleaned largely by reading between the lines of doctor’s perceptions of their views; they wanted methods that were simple and reliable, and they also were aware that these devices impacted their sexual behavior as well as their reproductive capacities.

Sketch of a diaphragm with spermicidal jelly and applicator. LeMon Clark, The Vaginal Diaphragm (St. Louis: C. V. Mosby, 1939), p. 9. Courtesy of the Kinsey Institute.
The politics of, controversy over, and subsequent rise of birth control clinics in the United States have been well documented.[3] The most widely prescribed method in those clinics and in private practice in the 1930s and 1940s was the diaphragm (aka Mensinga or Dutch pessary) in combination with spermicidal cream, foam, or jelly. The rise in popularity of the diaphragm in the 1930s was due to multiple factors, including a greater number of companies manufacturing them (including one that Margaret Sanger’s husband owned and operated); the loosening of laws against shipping sex-related materials and information after the Second Circuit Court of Appeals’ U.S. v. One Package ruling in 1936; the American Medical Association’s formal endorsement of contraceptives as medical devices in 1937; and the increased number of doctors learning contraceptive techniques in medical school.[4]
As Hannah M. Stone’s 1933 account of patients at her Newark, New Jersey clinic outlined, most patients did not come to the clinics knowing much about barrier methods or how to use them effectively. The most popular method that patients used before visiting the clinic was withdrawal, which had a 60 percent failure rate, or douching with a variety of dangerous and painful store-bought formulas (like Zonite or Lysol) and/or home preparations (like vinegar, soap, or salt), which both had a 42 percent failure rate. Those who already used condoms or diaphragms did not use them effectively, as Stone reported that users of both of those methods also had a 42 percent failure rate.[5]
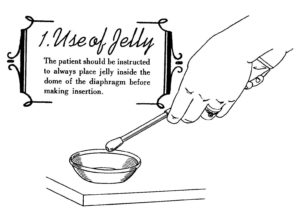
Sketch of a woman’s hand, with prominent engagement and wedding rings, demonstrating how to apply spermicidal jelly to a diaphragm. LeMon Clark, The Vaginal Diaphragm (St. Louis: C. V. Mosby, 1939), p. 17. Courtesy of the Kinsey Institute.
Stone prescribed the diaphragm for 1461 patients and tracked their progress through follow-up visits. After six months, 1110 of them (76 percent) had not become pregnant. Two hundred seventy-eight patients did not use the diaphragm because they were already pregnant during their first visit; the husband or the wife was ill or already sterilized; the patients objected because they had “no confidence” in the device or were “uncertain of technique”; they found the device uncomfortable or painful, too difficult, too much trouble; or the husband objected.[6] Clearly, the fact that patients had been fitted for diaphragms by a doctor and had had professional instruction regarding use and maintenance of the devices made a positive difference in their effectiveness. The anonymous author of the 1938 pamphlet The Fitting and Use of Diaphragms also asserted the necessity, indeed centrality, of doctors for contraceptive technology, as especially after giving birth, patients likely needed a different size device: “It is because of these varying conditions that a doctor’s services are necessary.”[7] Le Mon Clark hinted at the problems some of his fellow doctors had with patients learning to use contraception on their own: “to fulfill his duty and responsibility to the patient, the physician should point out that birth control is a most powerful force to be used most wisely and well. Brides should be cautioned against postponing pregnancy for too long a period of time.”[8]
Some husbands (any unmarried male partners went unmentioned) disliked cervical caps and diaphragms because their penises would bang against them if they thrust deeply.[9] Doctors and cap and diaphragm manufacturers (who, of course, had a profit motive) also wrote that these men often objected to condoms as well, on the grounds that they dulled sensation.[10] Manufacturers used men’s dislike of condoms as support for their argument that diaphragms promoted happiness in marriage: “It will relieve her marriage of that constantly recurring worry and bring to both husband and wife a new happiness, with an attendant improvement in health and efficiency for both.”[11]
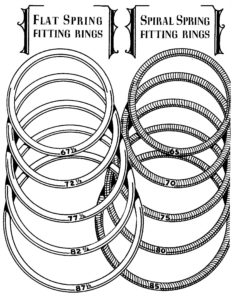
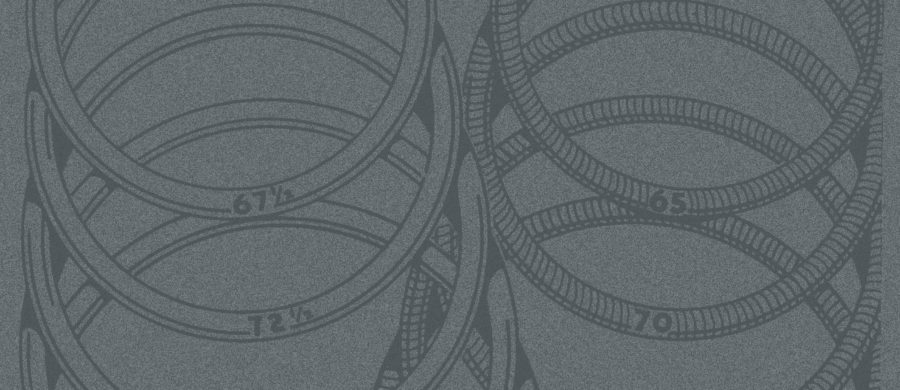
Sketch of diaphragm rings with different diameters. LeMon Clark, The Vaginal Diaphragm (St. Louis: C. V. Mosby, 1939), p. 23. Courtesy of the Kinsey Institute.
Beyond husbands’ complaints, only Robert Latou Dickinson and Ernst Grafenberg took women’s sexual desire and pleasure into account when considering the effectiveness of contraception. They mentioned that women were sometimes unable to have an orgasm while using the diaphragm. However, “because the cervix cap leaves the interior wall uncovered, whereas the diaphragm covers it, these patients can…orgasm after the change is made.” They used a glass tube in the size of the penis, “through which the action of its tip may be observed by inspection with a headlight. The tip passes alongside or behind the capped cervix.”[12] The doctor could then see if the device was oversized or perhaps misplaced, leading to discomfort for both partners. However, they could not use the device to observe how couples positioned themselves during sex, how long their sexual encounters lasted, and the relief they felt having sex with limited pregnancy risk—other elements important in considering how much pleasure both partners experienced.
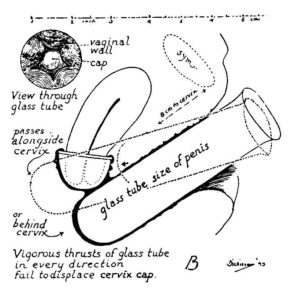
Robert L. Dickinson’s drawing of how he used a glass tube to mimic the thrusting of a penis to see if it displaced the cervical cap. Ernst Grafenberg and Robert L. Dickinson, “Conception Control by Plastic Cervix Cap,” Western Journal of Surgery, Obstetrics, and Gynecology 52 (August 1944): 339.
Doctors’ writings reflect an ambivalence regarding responsibility for the effectiveness of contraception but also their interest in putting contraceptive technology into women’s hands. As Grafenberg and Dickinson put it in 1944, “All protection against unwise pregnancy has as [its] primary desirability that the means be placed in the hands of the woman herself.”[13] Many doctors perceived that women’s attitudes toward a new technology and their intention to make it work counted more than academic intelligence as it related to effectiveness. Dickinson and Lura Beam, compiling records from Dickinson’s Brooklyn, New York practice in the early twentieth century, emphasized that “the couples who always used successful methods which failed with others, may have been only those who could follow directions exactly. Comparison fails to show that highly educated couples are more successful in controlling birth instruction than the less intelligent.”[14]
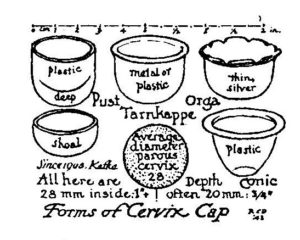
Robert L. Dickinson’s drawing of different types of cervical caps. Ernst Grafenberg and Robert L. Dickinson, “Conception Control by Plastic Cervix Cap,” Western Journal of Surgery, Obstetrics, and Gynecology 52 (August 1944): 339.
That was also the case on the West Coast. Dr. Nadina R. Kavinoky and Elizabeth U. Brown were staff members at a hospital for poor women in Pasadena, California funded by the Procter & Gamble heir Clarence Gamble. When prescribing a barrier method to a new patient, they noted that “an attempt is made to determine her emotional attitude toward sex and her own reproductive organs since her ability to learn the technique depends upon this rather than upon her basic intelligence.”[15] The author of The Fitting and Use of Diaphragms observed: “A patient’s primary interest in contraception centers around the question of reliability. After she has been fitted and instructed in the use of a diaphragm, the woman may inquire whether she can really put full reliance in that method. This should not be accepted as any reflection on the physician. It is merely a symptom of the extreme fear which has so long grasped the mind of that individual…. A few confident words of assurance are in order with all such patients.”[16]
On the other hand, Stone described the ambiguity she felt when reflecting on the failure rates for her patients: “Often enough…it is difficult to decide upon the exact cause of a failure in a particular case…. A patient will fail with a method which has been given her either because she does not follow instructions fully, and is careless in using it, or because her technic of applying the method is faulty, or else because the method as prescribed is inadequate to protect her against contraception.”[17] Clark alluded to the fact that doctors may be partially at fault if patients used a method incorrectly, and articulated his hope that his guidebook would help fellow practitioners: “this work may serve as a starting point for the elaboration of improvements in the technique of imparting information to patients in such a way as to help eliminate failure due to carelessness or misunderstanding—failure of the human element rather than failure of the method.”[18]
Barrier methods of contraception for women remained popular throughout the 1940s and 1950s, though their use diminished significantly after the U.S. Food and Drug Administration approved the hormonal pill for contraceptive purposes in 1960.[19] They became popular again in the late 1970s and early 1980s, as members of the American feminist health movement chronicled the problems of high-dose pills and conducted their own testing and advocacy of the cervical cap.[20] However, as manufacturers created lower-dose pills, more women began to use the pill again, and to date, it remains the most popular woman-controlled contraceptive technology in the U.S. along with female sterilization.[21] Cervical caps, diaphragms, and spermicides are all still manufactured but relatively difficult to find.
As Judy Wajcman noted, “the distinguishing insight of feminist STS or technofeminism is that gender is integral to this sociotechnical process: that the materiality of technology affords or inhibits the doing of particular gender power relations.”[22] The materiality of the cervical cap and diaphragm, as machine-manufactured, medically fitted devices, made a noticeable change in the lives of those who used them. These pamphlets and articles show that doctors did not entirely trust women with the responsibility for the careful use and maintenance of technology, and that they wanted to maintain some control over women’s contraceptive practices and attitudes toward pregnancy and childbirth. In turn, however, many women did not entirely trust doctors or the prescribed devices, and often supplemented or replaced prescription-only devices with their own douching solutions or trusted their husbands to withdraw in time. Some husbands disliked the feeling of any barrier method, whether male- or female-controlled, but offered no alternative of their own to control fertility aside from withdrawal. The wide availability of mass-produced, reliable contraceptive barrier methods highlighted the relationship between contraceptive use and sexual pleasure and shifted the landscape of heterosexual marriage—so that both partners could have a say in when sex was for pleasure, and when it was also for procreation.
At the same time, though, “changes in people’s relations to technology may take place without changes in the patterns of inequality.”[23] The availability of a technology alone could not in itself challenge inequality or gendered power relations within a marriage if the spouses did not change their feelings or behavior as a result. In the long run, barrier methods served as both symbols and materialities of how desires for pleasure and connection, with or without the possibility of pregnancy, structured heterosexual relationships.
Donna J. Drucker is Instructor of English for Special Purposes and Guest Lecturer at Technische Universität Darmstadt, Germany. She is the author of The Classification of Sex: Alfred Kinsey and the Organization of Knowledge which won the 2015 Bonnie and Vern L. Bullough Prize from the Foundation for the Scientific Study of Sexuality, and The Machines of Sex Research: Technology and the Politics of Identity 1945-1985. She writes regularly for the history of sexuality blog Notches and has articles forthcoming in 2017 from the Indiana Magazine of History and Information & Culture.
Suggested Readings
- Cathy Moran Hajo, Birth Control on Main Street: Organizing Clinics in the United States, 1919–1939 (Springfield: University of Illinois Press, 2010)
- Norman E. Himes, Medical History of Contraception (1936; New York: Schocken Books, 1970)
- Rose Holz, The Birth Control Clinic in a Marketplace World (Rochester: University of Rochester Press, 2014)
- Christina Simmons, Making Marriage Modern: Women’s Sexuality from the Progressive Era to World War II (New York: Oxford University Press, 2009)
- Andrea Tone, Devices and Desires: A History of Contraception in America (New York: Hill & Wang, 2001)
[1] Judy Wajcman, “Feminist Theories of Technology,” Cambridge Journal of Economics 34:1 (2010): 143–152, esp. 144.
[2] See for example, Norman Carr [pseud.], Marriage Hygiene: As Prescribed by Physicians (Chicago: Medical Bureaus of Information, 1937).
[3] See for example, Cathy Moran Hajo, Birth Control on Main Street: Organizing Clinics in the United States, 1919–1939 (Springfield: University of Illinois Press, 2010) and Rose Holz, The Birth Control Clinic in a Marketplace World (Rochester: University of Rochester Press, 2014).
[4] Andrea Tone, Devices & Desires: A History of Contraceptives in America (New York: Hill & Wang, 2001), 127, 134–135, 177; United States v. One Package, 86 F. 2d 737 – Circuit Court of Appeals, 2nd Circuit 1936.
[5] Hannah M. Stone, Maternal Health and Contraception: A Study of 2,000 Patients from the Maternal Health Center, Newark, N.J. (n.p.: Medical Journal and Record, 1933), 8.
[6] Stone, Maternal Health and Contraception, 16.
[7] Anonymous, The Fitting and Use of Diaphragms (n.p.: C.B. Hagaman, 1938), 5.
[8] Le Mon Clark, The Vaginal Diaphragm: Its Fitting and Use in Contraceptive Technique (St. Louis: C. V. Mosby, 1939), 105.
[9] Anonymous, Fitting and Use of Diaphragms, 11; Nadina R. Kavinoky and Elizabeth U. Brown, “The Necessity of Repeated Examinations in the Fitting of Contraceptive Diaphragms,” Western Journal of Surgery, Obstetrics, and Gynecology 51 (April 1943): 140–142, esp. 140; Ernst Grafenberg and Robert L. Dickinson, “Conception Control by Plastic Cervix Cap,” Western Journal of Surgery, Obstetrics, and Gynecology 52 (August 1944): 335–340, esp. 338.
[10] Carr, Marriage Hygiene, 9.
[11] Ibid., 20.
[12] Grafenberg and Dickinson, “Conception Control by Plastic Cervix Cap,” 338, 339. Using a glass tube to observe the interior of the vagina prefigured William H. Masters and Virginia Johnson’s use of a Plexiglas dildo-camera to record cervical movements during sexual stimulation. See William H. Masters and Virginia E. Johnson, Human Sexual Response (Boston: Little, Brown, 1966).
[13] Grafenberg and Dickinson, “Conception Control by Plastic Cervix Cap,” 335.
[14] Robert Latou Dickinson and Lura Beam, A Thousand Marriages (Baltimore: Williams & Wilkins, 1931), 217.
[15] Kavinoky and Brown, “Necessity of Repeated Examinations in the Fitting of Contraceptive Diaphragms,” 140.
[16] Anonymous, Fitting and Use of Diaphragms, 17.
[17] Stone, Maternal Health and Contraception, 24.
[18] Clark, Vaginal Diaphragm, 7.
[19] Elaine Tyler May, America + the Pill: A History of Promise, Peril, and Liberation (New York: Basic Books, 2011).
[20] Donna J. Drucker, “The Cervical Cap in the Feminist Women’s Health Movement, 1976–1978,” Notches: (Re)Marks on the History of Sexuality. <http://notchesblog.com/2016/03/24/the-cervical-cap-in-the-feminist-womens-health-movement-1976-1988>. Accessed 26 August 2016.
[21] Guttmacher Institute, “Contraceptive Use in the United States.” <https://www.guttmacher.org/fact-sheet/contraceptive-use-united-states>. Accessed 29 August 2016.
[22] Wajcman, “Feminist Theories of Technology,” 150.
[23] Anne-Jorunn Berg and Merete Lie, “Feminism and Constructivism: Do Artifacts Have Gender?,” Science, Technology, & Human Values 20 (Summer 1995): 332-351, esp. 342.
